Ideal Protein Overview
The Ideal Protein Protocol is a medically developed and nutritionally balanced Protocol designed to help patients lose weight and better manage their health.
Ideal Protein Overview
The Ideal Protein Protocol is a medically developed and nutritionally balanced Protocol designed to help patients lose weight and better manage their health.
Proven Weight Loss and Improved Metabolic Health
View our collection of clinical trials, case studies and peer-reviewed research.
TULANE UNIVERSITY:
“Effect of Ideal Protein versus low-fat diet for weight loss: A randomized controlled trial”
A new, peer-reviewed study published in Obesity Science & Practice, led by Tulane University, compared the Ideal Protein dietary behavioral intervention (IP system) to a standard, guideline-based, low-calorie, low-fat (LCLF) dietary behavioral intervention.¹·²
The 3-month trial assigned 192 adult participants with body mass index (BMI) ≥30 and ≤49 kg/m2, to either the Ideal Protein Phase 1 diet or LCLF diet interventions.¹
Reported Primary Endpoint (body weight):
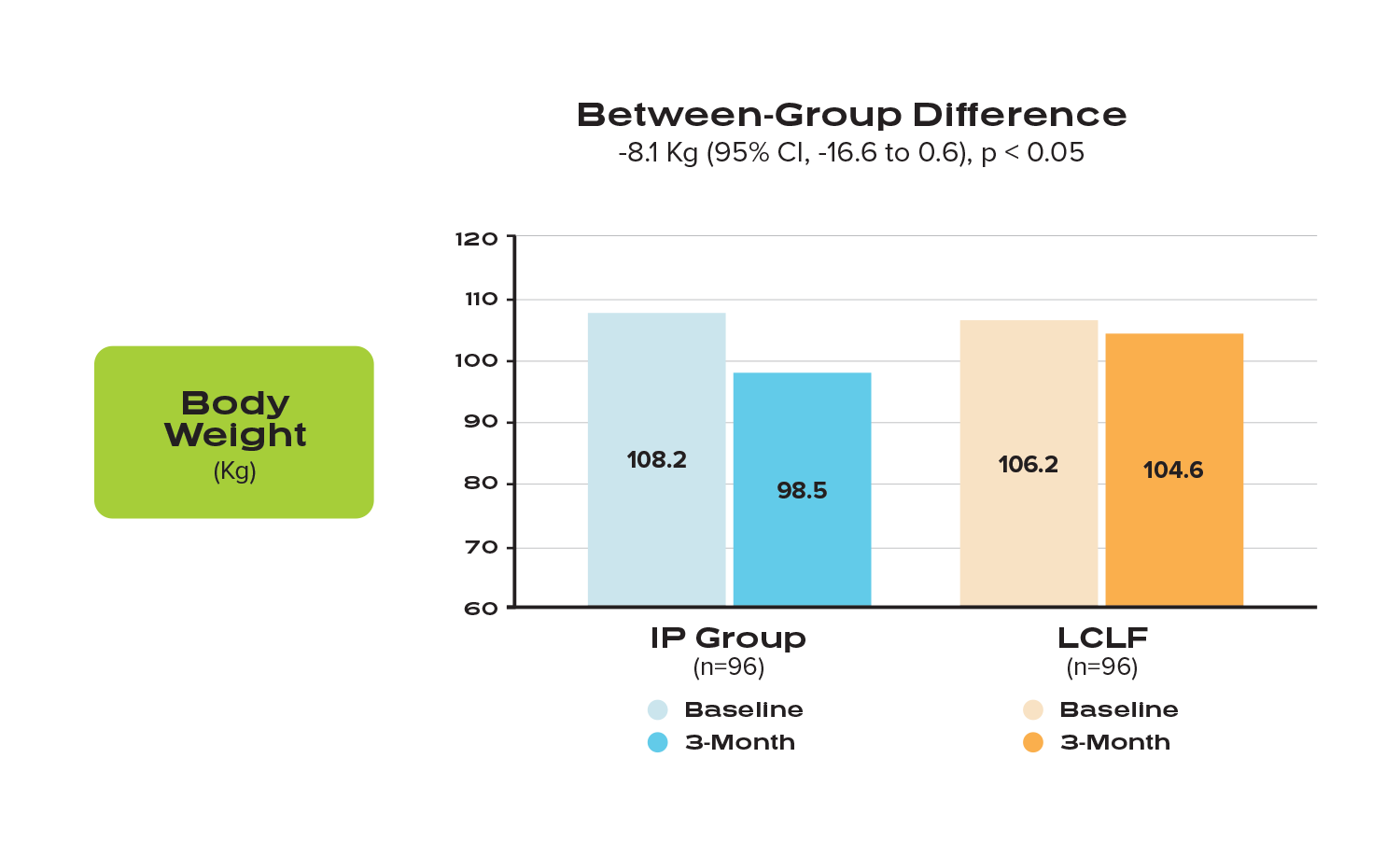
“The IP system resulted in statistically significant greater weight loss among men and women with obesity and additional risk factors for cardiovascular disease (CVD).” ¹
(Comparison of mean weight loss in kg between participants in the IP group vs the LCLF group, at 3 months). Clustered column graph depicting average weight at baseline and 3-month follow-up for each dietary intervention group, respectively.
Reported Secondary Endpoints:
Although both groups saw improvements in several cardiometabolic risk factors, there were significant between-group differences favoring the IP Group, which “experienced greater improvements in waist and hip circumference, total cholesterol, and triglycerides.”¹
Results of the remaining secondary outcomes for the IP group were equal to or exhibited more favorable trends than the LCLF group, although some did not reach statistical significance in either group.
The study concludes that “this 3-month randomized, parallel group trial showed that the IP system resulted in greater weight loss and reduction in several CVD risk factors than a guideline-based LCLF dietary behavioral intervention among black and white adults with obesity and additional CVD risk factors. Thus, the IP system appears to be a safe and efficacious way to lose weight and reduce CVD risk factors among men and women with obesity and additional CVD risk factors. Further research is warranted to examine outcomes over the longer term.”¹𝄒²
Funding was provided by a grant from Ideal Protein Laboratories COP Inc, Quebec, Canada to Tulane University, School of Public Health and Tropical Medicine.
¹Fernandez CA, Potts K, Bazzano LA. Effect of ideal protein versus low-fat diet for weight loss: a randomized controlled trial. Obes Sci Pract. 2021; 1- 9. doi:10.1002/osp4.567
² Jensen MD, et.al.. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63:2985-3023.
UNIVERSITY OF BRITISH COLUMBIA:
“A randomized controlled trial of pharmacist-led therapeutic carbohydrate and energy restriction in type 2 diabetes”
A recent randomized, controlled clinical study, led by the University of British Columbia and sponsored by the Institute for Personalized Therapeutic Nutrition, evaluates the impact of a Pharmacist-led therapeutic carbohydrate restricted diet (Pharm-TCR) on type 2 diabetes (T2D). Participants in the Pharm-TCR group were asked to follow the Ideal Protein weight loss diet plan, supplemented with whole foods.¹
The primary objective of the study, published in Nature Communications, was to determine if a Pharm-TCR diet can safely reduce and/or eliminate the use of glucose-lowering medications and lead to improvements in A1C, body composition, cardiometabolic health, and quality of life.² Of the 188 patients that participated in the 12-week study, 98 patients followed a Pharm-TCR diet, and 90 patients received treatment-as-usual.*
Reported Primary Outcomes for Pharm TCR patients after 12 weeks
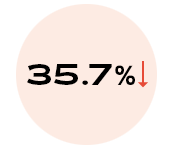
of patients experienced discontinuation of glucose lowering medication (p < 0.0001)
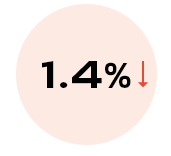
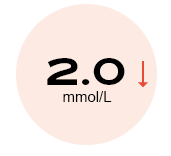
reduction in A1C
(p < 0.0001)
SECONDARY OUTCOMES:
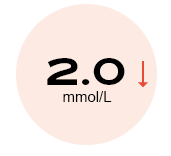
reduction in fasting plasma
glucose (p < 0.0001)

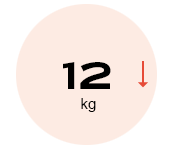
reduction in
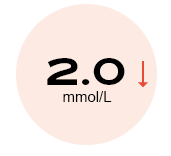
triglycerides (p < 0.0001)
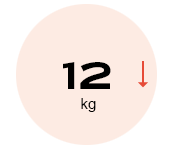
reduction in total body
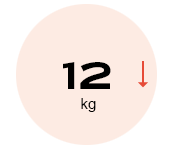
weight* (p < 0.0001)
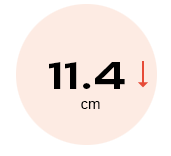
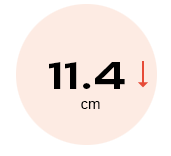
reduction in waist
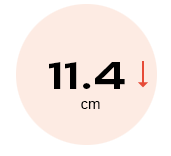
circumference (p < 0.0001)
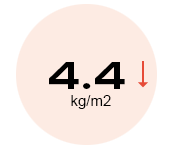
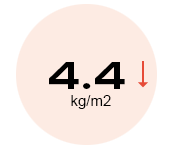
reduction in BMI (p < 0.0001)
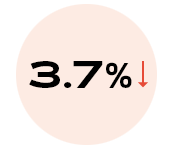
reduction in body fat
percentage (p < 0.0001)
reduction in fasting plasma
glucose (p < 0.0001)

reduction in
triglycerides (p < 0.0001)
reduction in total body
weight* (p < 0.0001)
reduction in waist
circumference (p < 0.0001)
reduction in BMI (p < 0.0001)
reduction in body fat
percentage (p < 0.0001)
As stated in the 2019 Diabetes Care report, “low-carbohydrate eating patterns, especially very low-carbohydrate (VLC) eating patterns, have been shown to reduce A1C and the need for antihyperglycemic medications.”³
*Treatment-as usual defined as: given information pamphlets on diet and lifestyle conforming with 2013 Diabetes Canada (formerly the Canadian Diabetes Association) Clinical Practice Guidelines.
¹ Durrer, C., McKelvey, S., Singer, J. et al. A randomized controlled trial of pharmacist-led therapeutic carbohydrate and energy restriction in type 2 diabetes. Nat Commun 12, 5367 (2021). https://doi.org/10.1038/s41467-021-25667-4
² Durrer, C., McKelvey, S., Singer, J. et al. Pharmacist-led therapeutic carbohydrate restriction as a treatment strategy for type 2 diabetes: the Pharm-TCR randomized controlled trial protocol. Trials 20, 781 (2019). https://doi.org/10.1186/s13063-019-3873-7
³ Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, MacLeod J, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. (2019) 42:731–54. doi: 10.2337/dci19-0014
NORTHSHORE UNIVERSITY HEALTH SYSTEM:
“Ketogenic, Hypocaloric Diet Improves Nonalcoholic Steatohepatitis”
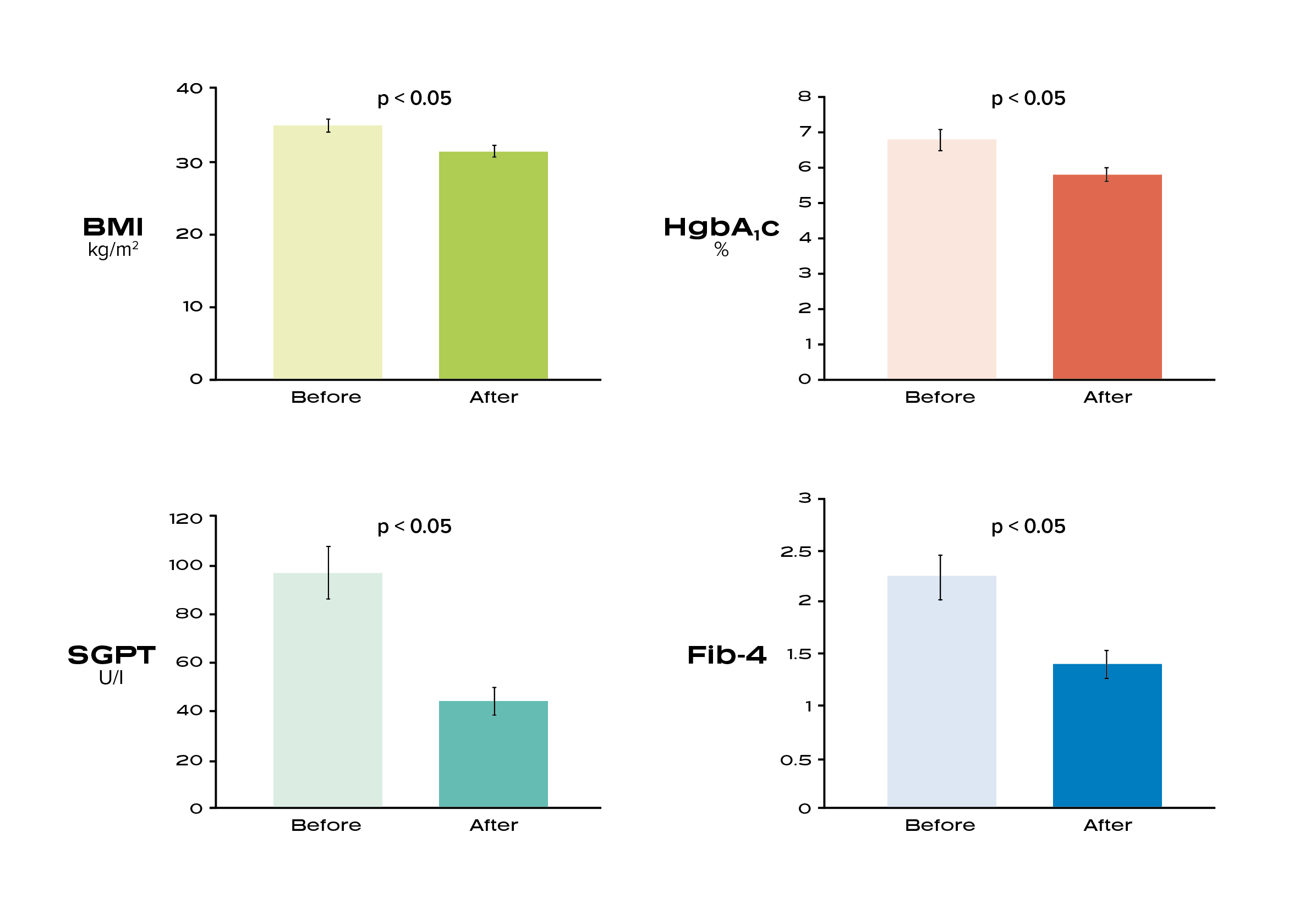
The goal of this study was to examine the impact of the Ideal Protein Protocol on metabolic parameters and markers of liver disease in patients with non-alcoholic steatohepatitis.
The findings highlight the beneficial effects of the Ideal Protein Protocol on liver enzymes and a marker of liver fibrosis among a group of patients with NASH⁸’⁹
Experts estimate that the prevalence of NASH is up to 12%, over 16 million US adults, with estimates of a 63% increase by year 2030. ¹⁰
⁸ Belopolsky Y, Khan MQ, Sonnenberg A, Davidson DJ, Fimmel CJ. Ketogenic, Hypocaloric Diet Improves Nonalcoholic Steatohepatitis. J Transl Int Med. 2020;8(1):26-31. Published 2020 May 9. doi:10.2478/jtim-2020-0005
⁹ Promrat K, Kleiner DE, Niemeier HM, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010;51(1):121-129. doi:10.1002/hep.23276
¹⁰ Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67(1):123-133. doi:10.1002/hep.29466
Dr. Davidson is a member of Ideal Protein’s Medical Advisory Board.
AVERA CANCER INSTITUTE:
Inflammation & Heart Health
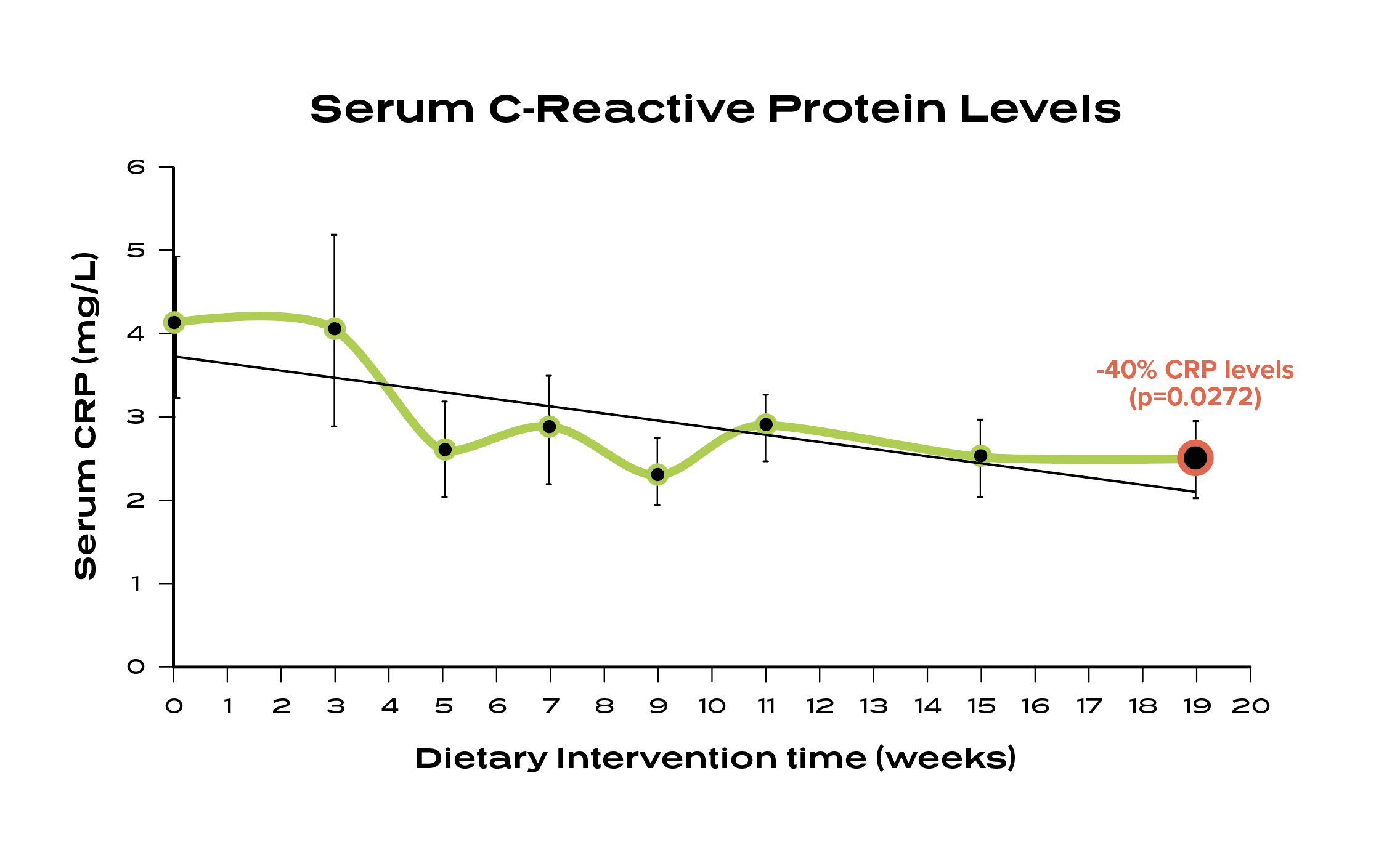
A 19-week study with the Avera Cancer Institute reported a 40% reduction in C-reactive protein for patients who completed the Ideal Protein Protocol. The study also reported a rapid decline in resting fasting insulin and a mean weight loss of 19.9% body fat. ⁶
Studies show increased CRP levels are associated with a higher risk for inflammatory conditions. ⁷
⁶ Bohlen, Krista & Krie, Amy & Hu, Yueshan & Ageton, Cheryl & Nickles, Heidi & Norfolk, Daniel & Kittelsrud, Julie & Thomes, Reggie & Fahrendorf, Adam & Muth, Jessica & Rojas-Espaillat, Luis & Davies, Gareth. (2013). Low Carbohydrate Dietary Intervention Improves Insulin, Hormonal Levels and Inflammatory Markers in Early Stage, Postmenopausal Breast Cancer Survivors. Cancer Research. 73. 10.1158/0008-5472.SABCS13-PD2-5.
⁷ Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;112(2):299. doi:10.1172/JCI200318921C
ASPIRUS HEALTH:
3-year Weight Maintenance & Healthcare Savings

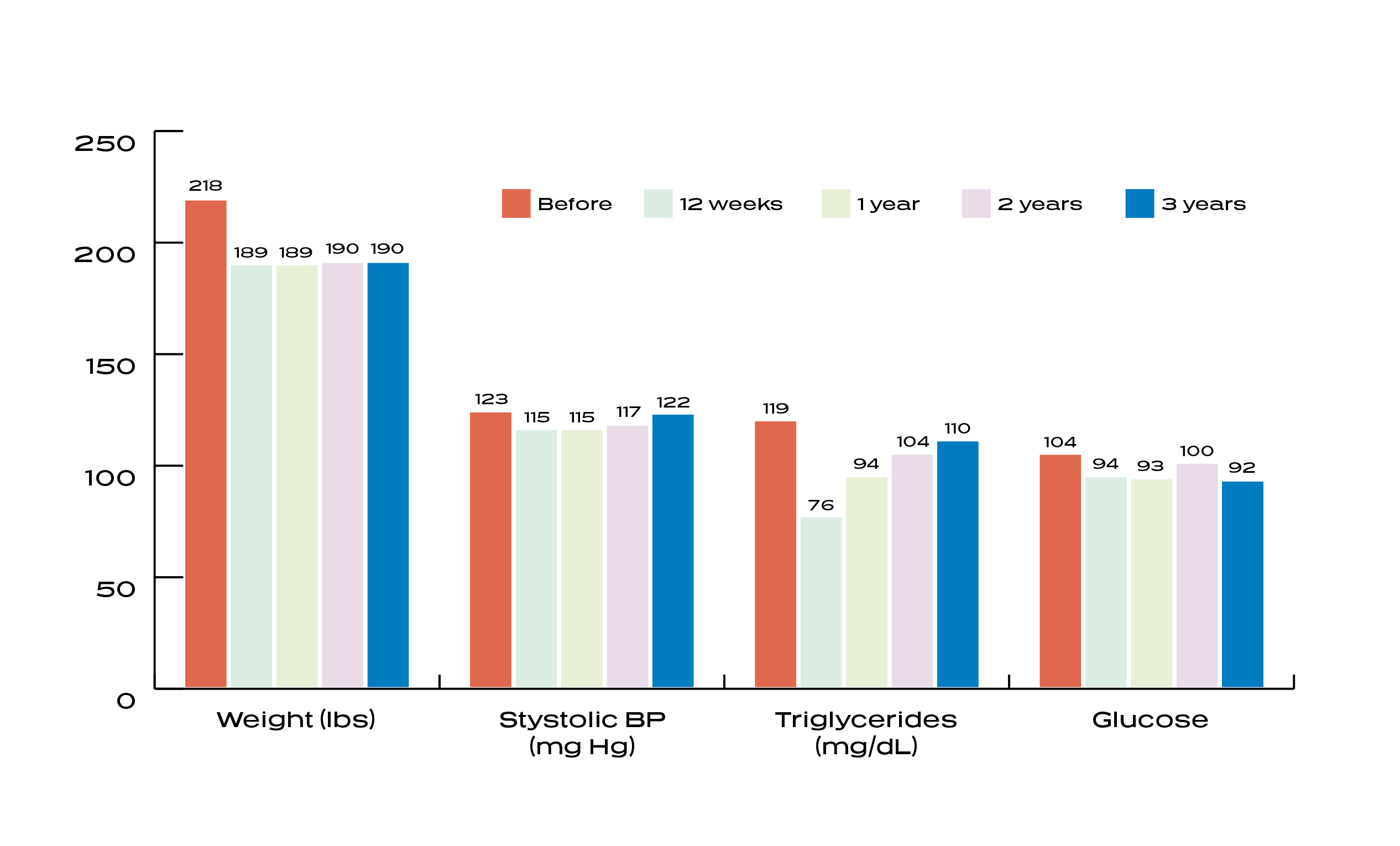
A study conducted by Aspirus, reported that after 3 years, participants who completed the Ideal Protein Protocol maintained an average weight loss of 12.8%, resulting in an 18% reduction in overall average claim care costs, saving an average of $916.97 per participant, per year. ²
A study published by The American Journal of Clinical Nutrition reports that if individuals can succeed at maintaining their weight loss for 2 or more years, they can reduce their risk of subsequent regain by nearly 50%.³
² Effect of The Ideal Protein Weight Loss Protocol on Employee Health Care Costs, By: Timothy Logemann, MD; David K. Murdock, MD; Kelly O’Heron, RD
³ Rena R Wing, Suzanne Phelan, Long-term weight loss maintenance, The American Journal of Clinical Nutrition, Volume 82, Issue 1, July 2005, Pages 222S, 225S, https://doi.org/10.1093/ajcn/82.1.222S
ASPIRUS HEALTH:
“Effect of the Ideal Protein Weight Loss Method on Weight Loss and Metabolic Parameters”
According to a study conducted and published by Aspirus, an eight-hospital health system in Wisconsin and Michigan, entitled Effect of the Ideal Protein Weight Loss Method on Weight Loss and Metabolic Parameters,¹ 233 patients completed at least 12 weeks of the Protocol. The 12-week results were presented at the Cleveland Clinic’s 9th Annual Obesity Summit and at the Annual Scientific Meeting of the National Obesity Society.
Our peer-reviewed, published research demonstrates that, among patients who completed the study, metabolic health can be improved in as little as 12 weeks.
15%↓
BMI
8.6%↓
Blood
Pressure
14%↓
Total Body Weight*
14%↓
Cholesterol
86%
Dieter
Compliance
14%↓
Fasting
Glucose
45%↓
Triglycerides
13%↓
LDL
Study Concludes: The Ideal Protein Protocol produces improvements in blood pressure, lipid profile, particularly in regard to triglyceride levels and fasting glucose levels. The findings suggest that due to the successful weight loss reported, the Protocol could help with cardiovascular risk.
* Total Body Weight -3.5lbs/wk for men and -2.4lbs./wk for women
¹ Effect of the Ideal Protein Weight Loss Method on Weight Loss and Metabolic Parameters By: Timothy Logemann, MD; David K. Murdock, MD, MS; Kelly O’Heron, RD & Adam Hoffmann
IDEAL PROTEIN:
Robust Weight Loss with Lean Mass Preserved
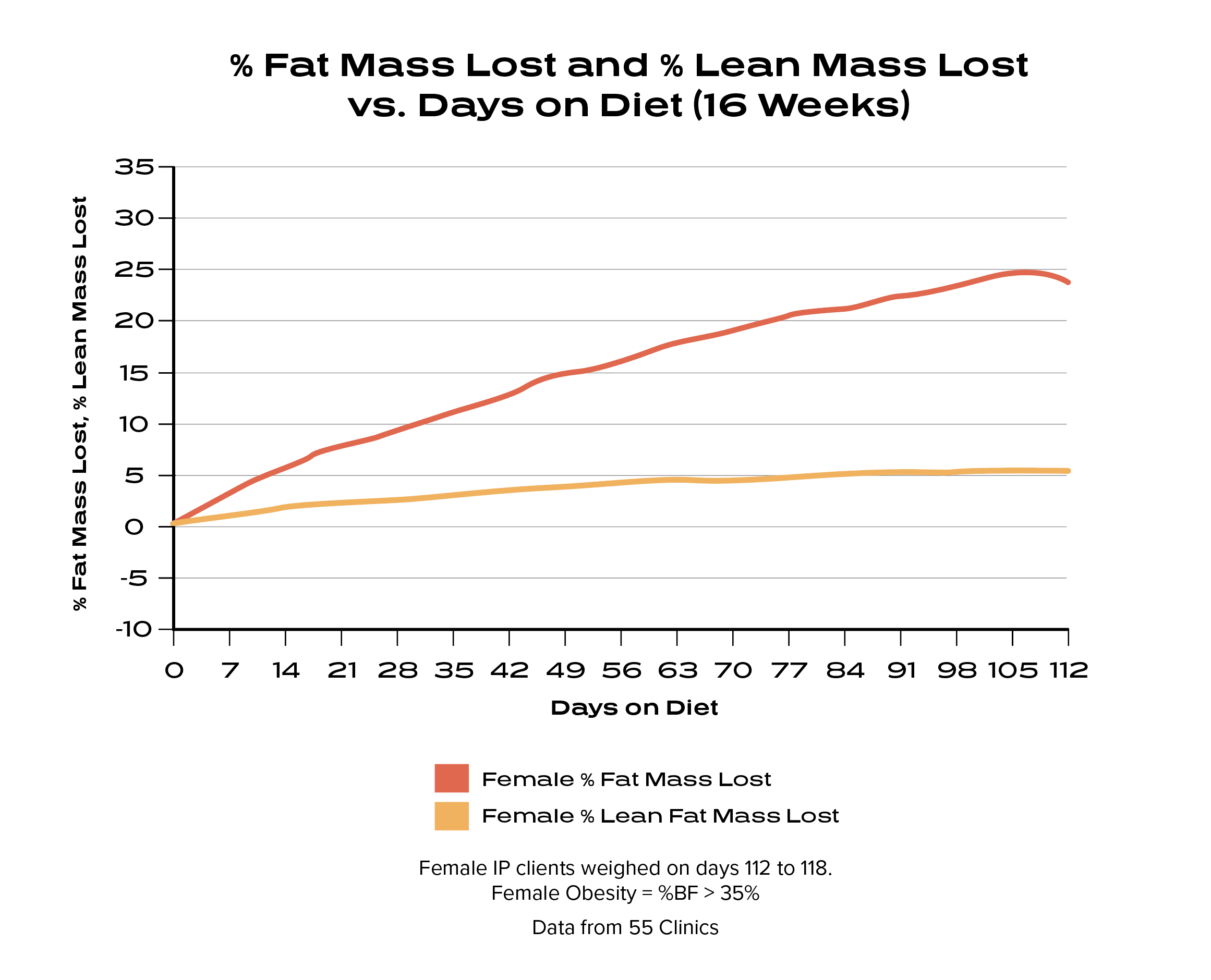
After 16 weeks on the Ideal Protein Protocol, males lost an average of 25% fat mass while preserving 98% lean body mass and females lost an average 24% of fat mass while preserving 95% lean body mass.⁴
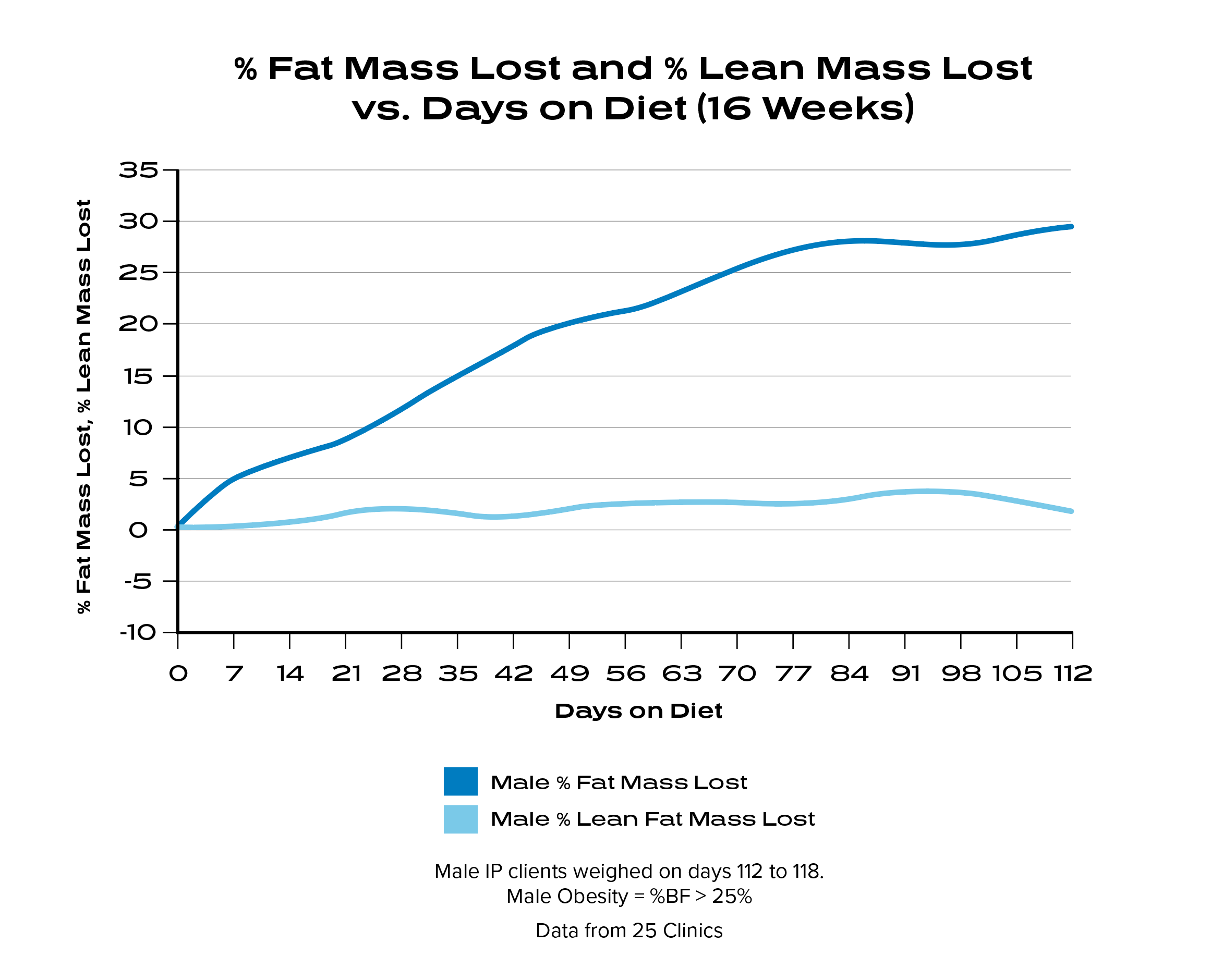
A 2014 Obesity Review states: “Maximizing fat loss while preserving lean tissue mass and function is a central goal of modern obesity treatments. A widely cited rule guiding expected loss of lean tissue as fat-free mass (FFM) states that approximately one-fourth of weight loss will be FFM (i.e. ΔFFM/ΔWeight = ∼0.25), with the remaining three-fourths being fat mass.” 5
⁴ Frank Douglis, MD, Ideal Protein Data Analysis, 2016.
⁵ Heymsfield SB, Gonzalez MC, Shen W, Redman L, Thomas D. Weight loss composition is one-fourth fat-free mass: a critical review and critique of this widely cited rule. Obes Rev. 2014;15(4):310-321. doi:10.1111/obr.12143
Dr. Douglis is an Executive Medical Board Member and Chief Medical Advisor for Ideal Protein.
The Ideal Protein Difference
The Ideal Protein Protocol is a medically developed weight loss and maintenance program featuring individualized, professional health coaching. Our Stabilization and Maintenance Phases give patients the support they need for long-term success.
Proprietary Weight
Loss Protocol
One-On-One
Coaching
Food &
Supplements
Proprietary Weight Loss Protocol
Ideal Protein is a structured three-phase Protocol designed for long-term weight maintenance. The Weight Loss phase is designed to optimize fat loss through nutritional ketosis, a safe and natural metabolic state in which the body’s primary fuel source is coming from ketone bodies – energy molecules produced by “burning fat.”
Throughout the Weight Loss Phase, lean body mass is preserved through the intake of partial meal replacements, which contain protein of high biological value.
One-on-One Coaching
Studies show that to lose and sustain weight loss successfully, there is nothing more important than being assisted by a qualified coach.¹ All coaches are provided ongoing training from Ideal Protein. Through behavior modification and education, our coaches help empower patients with strategies that are critical for long-term healthy weight maintenance.
¹ Sforzo GA, Kaye MP, Todorova I, et al. Compendium of the Health and Wellness Coaching Literature. Am J Lifestyle Med. 2017;12(6):436-447. Published 2017 May 19. doi:10.1177/1559827617708562
Food and Supplements
The Ideal Protein Protocol combines whole foods with medically designed partial meal replacements. Lean body mass is preserved through an adequate daily intake of high biological protein. Essential nutrients are provided through daily supplements, water, and low-glycemic vegetables. Our products are FDA label approved and meet the Recommended Daily Allowance (RDA) standards for all macro food groups and micro nutritional needs.
Stabilization and Maintenance Plans
Following the Weight Loss Phase (Phase 1), the body’s biological response seeks to regain lost energy stores. The Protocol reduces this response through the Stabilization phase by adjusting macronutrient intake in the right proportions to effectively manage hunger, promote greater satiety, and maintain weight loss.
During the 12-month Maintenance phase, patients continue to receive ongoing education, support, and strategies from their coach and clinic to maintain their weight loss and daily navigate an extensive food landscape.
Medical Advisory Board
Ideal Protein’s Medical Advisory Board — comprised of highly regarded medical physicians and industry experts in obesity — provides guidance to healthcare providers who share the same goal of fighting the obesity epidemic through metabolic transformation.
Widely Distributed by Healthcare Providers
Thousands of healthcare providers across North America offer and recommend Ideal Protein to patients, helping them naturally gravitate to a healthy weight and improved metabolic state.
Stabilization and
Maintenance Plans
Medical Advisory
Board
Widely Distributed by
Healthcare Providers
Proprietary Weight Loss Protocol
Proprietary Weight Loss Protocol
Ideal Protein is a structured three-phase Protocol designed for long-term weight maintenance. The Weight Loss phase is designed to optimize fat loss through nutritional ketosis, a safe and natural metabolic state in which the body’s primary fuel source is coming from ketone bodies – energy molecules produced by “burning fat.”
Throughout the Weight Loss Phase, lean body mass is preserved through the intake of partial meal replacements, which contain protein of high biological value.
One-On-One Coaching
One-on-One Coaching
Studies show that to lose and sustain weight loss successfully, there is nothing more important than being assisted by a qualified coach.¹ All coaches are provided ongoing training from Ideal Protein. Through behavior modification and education, our coaches help empower patients with strategies that are critical for long-term healthy weight maintenance.
¹ Sforzo GA, Kaye MP, Todorova I, et al. Compendium of the Health and Wellness Coaching Literature. Am J Lifestyle Med. 2017;12(6):436-447. Published 2017 May 19. doi:10.1177/1559827617708562
Food & Supplements
Food and Supplements
The Ideal Protein Protocol combines whole foods with medically designed partial meal replacements. Lean body mass is preserved through an adequate daily intake of high biological protein. Essential nutrients are provided through daily supplements, water, and low-glycemic vegetables. Our products are FDA label approved and meet the Recommended Daily Allowance (RDA) standards for all macro food groups and micro nutritional needs.
Stabilization and Maintenance Plans
Stabilization and Maintenance Plans
Following the Weight Loss Phase (Phase 1), the body’s biological response seeks to regain lost energy stores. The Protocol reduces this response through the Stabilization phase by adjusting macronutrient intake in the right proportions to effectively manage hunger, promote greater satiety, and maintain weight loss.
During the 12-month Maintenance phase, patients continue to receive ongoing education, support, and strategies from their coach and clinic to maintain their weight loss and daily navigate an extensive food landscape.
Medical Advisory Board
Medical Advisory Board
Ideal Protein’s Medical Advisory Board — comprised of highly regarded medical physicians and industry experts in obesity — provides guidance to healthcare providers who share the same goal of fighting the obesity epidemic through metabolic transformation.
Widely Distributed by Healthcare Providers
Widely Distributed by Healthcare Providers
Thousands of healthcare providers across North America offer and recommend Ideal Protein to patients, helping them naturally gravitate to a healthy weight and improved metabolic state.
A Turnkey Solution
Ideal Protein is a business-ready solution providing ongoing support for your patients, your coaches, and your business. We can help you improve patient health, better respond to pay-for-performance initiatives, and generate additional revenue.
Patient Support
Comprehensive solution for patients who struggle with weight issues
One-on-one coaching, behavior modification, and education
Stabilization and Maintenance Programs
The Ideal Protein App and Scale
Coaching Support
Ongoing training and education for coach and staff
The Ideal Protein Academy
Scientific Support Center
Robust patient support collateral
Virtual platform to support patients
Business Support
Dedicated Client Engagement Manager
New billable revenue and profit stream
Cost-effective use of existing staff resources
Efficient, well-developed program with no cost for implementation
Marketing collateral to promote your business
Business development plan
Testimonials
Hear what other Healthcare Providers and Practitioners are saying about Ideal Protein.*

Referrals
If you are interested in referring a patient to one of our existing Clinic Partner locations, please contact clientrelations@idealprotein.com. In accordance to the HIPAA Privacy Rule, please do not include any patient health information in your inquiry.
Learn more about partnering with Ideal Protein
If you are not a healthcare provider and are interested in learning more about Ideal Protein for yourself, please visit our main locations page.
"*" indicates required fields
*Any improvements in markers of health are attributed to resulting weight loss, not to the use of the Ideal Protein Protocol. Typical results vary up to 6 and 8 pounds lost during the first two weeks and up to 2 pounds per week thereafter when the Ideal Protein Weight Loss Protocol is followed properly.
Statements and testimonials made herein are not those of Ideal Protein, but of the individuals and entities cited as sources. Statements are made by physicians who own and operate clinics that offer the Ideal Protein Protocol and sell Ideal Protein products.
Testimonials, reference and/or results do not guarantee or predict future results, and you should not specifically expect to experience these results. Individual experiences while following the Ideal Protein Protocol are unique and may vary for each individual dieter. Dieters should consult their physician or other health care professional before starting the Ideal Protein Protocol or any other weight loss program to determine if it is right for their needs.
A new, peer-reviewed study published in Obesity Science & Practice, led by Tulane University, compared the Ideal Protein dietary behavioral intervention (IP system) to a standard, guideline-based, low-calorie, low-fat (LCLF) dietary behavioral intervention.¹·²
The 3-month trial assigned 192 adult participants with body mass index (BMI) ≥30 and ≤49 kg/m2, to either the Ideal Protein Phase 1 diet or LCLF diet interventions.¹
Reported Primary Endpoint (body weight):
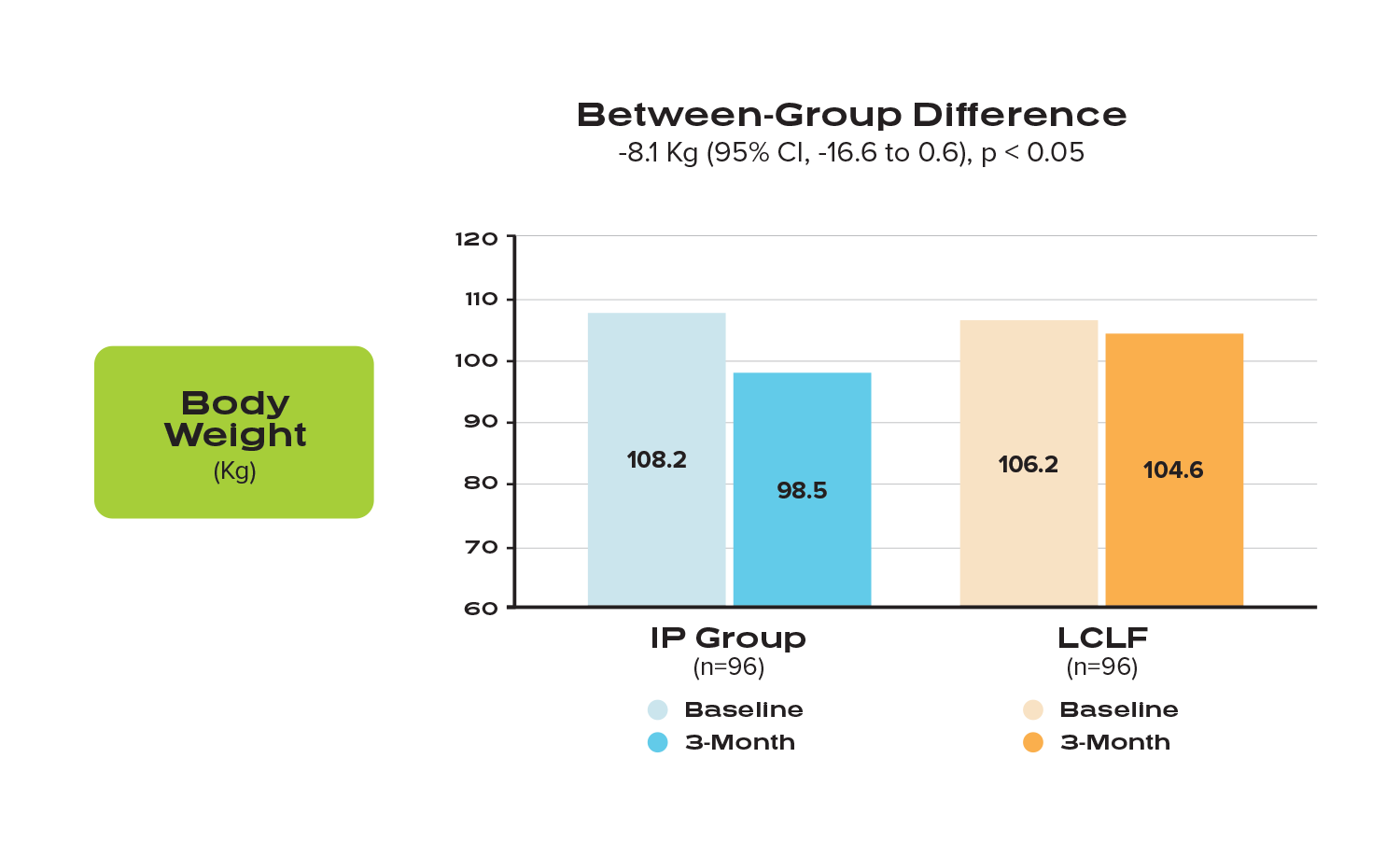
“The IP system resulted in statistically significant greater weight loss among men and women with obesity and additional risk factors for cardiovascular disease (CVD).” ¹
(Comparison of mean weight loss in kg between participants in the IP group vs the LCLF group, at 3 months). Clustered column graph depicting average weight at baseline and 3-month follow-up for each dietary intervention group, respectively.
Reported Secondary Endpoints:
Although both groups saw improvements in several cardiometabolic risk factors, there were significant between-group differences favoring the IP Group, which “experienced greater improvements in waist and hip circumference, total cholesterol, and triglycerides.”¹
Results of the remaining secondary outcomes for the IP group were equal to or exhibited more favorable trends than the LCLF group, although some did not reach statistical significance in either group.
The study concludes that “this 3-month randomized, parallel group trial showed that the IP system resulted in greater weight loss and reduction in several CVD risk factors than a guideline-based LCLF dietary behavioral intervention among black and white adults with obesity and additional CVD risk factors. Thus, the IP system appears to be a safe and efficacious way to lose weight and reduce CVD risk factors among men and women with obesity and additional CVD risk factors. Further research is warranted to examine outcomes over the longer term.”¹𝄒²
Funding was provided by a grant from Ideal Protein Laboratories COP Inc, Quebec, Canada to Tulane University, School of Public Health and Tropical Medicine.
¹Fernandez CA, Potts K, Bazzano LA. Effect of ideal protein versus low-fat diet for weight loss: a randomized controlled trial. Obes Sci Pract. 2021; 1- 9. doi:10.1002/osp4.567
² Jensen MD, et.al.. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63:2985-3023.
A recent randomized, controlled clinical study, led by the University of British Columbia and sponsored by the Institute for Personalized Therapeutic Nutrition, evaluates the impact of a Pharmacist-led therapeutic carbohydrate restricted diet (Pharm-TCR) on type 2 diabetes (T2D). Participants in the Pharm-TCR group were asked to follow the Ideal Protein weight loss diet plan, supplemented with whole foods.¹
The primary objective of the study, published in Nature Communications, was to determine if a Pharm-TCR diet can safely reduce and/or eliminate the use of glucose-lowering medications and lead to improvements in A1C, body composition, cardiometabolic health, and quality of life.² Of the 188 patients that participated in the 12-week study, 98 patients followed a Pharm-TCR diet, and 90 patients received treatment-as-usual.*
Reported Primary Outcomes for Pharm TCR patients after 12 weeks
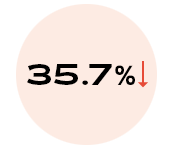
of patients experienced discontinuation of glucose lowering medication (p < 0.0001)
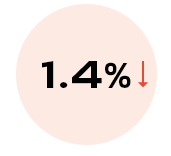
reduction in A1C
(p < 0.0001)
SECONDARY OUTCOMES:
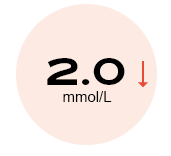
reduction in fasting plasma
glucose (p < 0.0001)

reduction in
triglycerides (p < 0.0001)
reduction in total body
weight* (p < 0.0001)
reduction in waist
circumference (p < 0.0001)
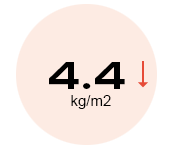
reduction in BMI (p < 0.0001)
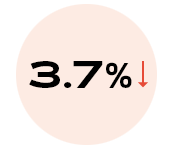
reduction in body fat
percentage (p < 0.0001)
reduction in fasting plasma
glucose (p < 0.0001)

reduction in
triglycerides (p < 0.0001)
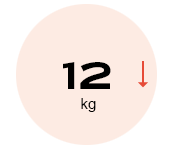
reduction in total body
weight* (p < 0.0001)
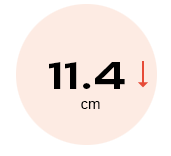
reduction in waist
circumference (p < 0.0001)
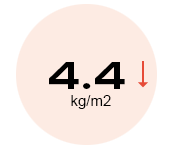
reduction in BMI (p < 0.0001)
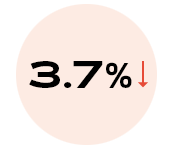
reduction in body fat
percentage (p < 0.0001)
As stated in the 2019 Diabetes Care report, “low-carbohydrate eating patterns, especially very low-carbohydrate (VLC) eating patterns, have been shown to reduce A1C and the need for antihyperglycemic medications.”³
*Treatment-as usual defined as: given information pamphlets on diet and lifestyle conforming with 2013 Diabetes Canada (formerly the Canadian Diabetes Association) Clinical Practice Guidelines.
¹ Durrer, C., McKelvey, S., Singer, J. et al. A randomized controlled trial of pharmacist-led therapeutic carbohydrate and energy restriction in type 2 diabetes. Nat Commun 12, 5367 (2021). https://doi.org/10.1038/s41467-021-25667-4
² Durrer, C., McKelvey, S., Singer, J. et al. Pharmacist-led therapeutic carbohydrate restriction as a treatment strategy for type 2 diabetes: the Pharm-TCR randomized controlled trial protocol. Trials 20, 781 (2019). https://doi.org/10.1186/s13063-019-3873-7
³ Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, MacLeod J, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. (2019) 42:731–54. doi: 10.2337/dci19-0014
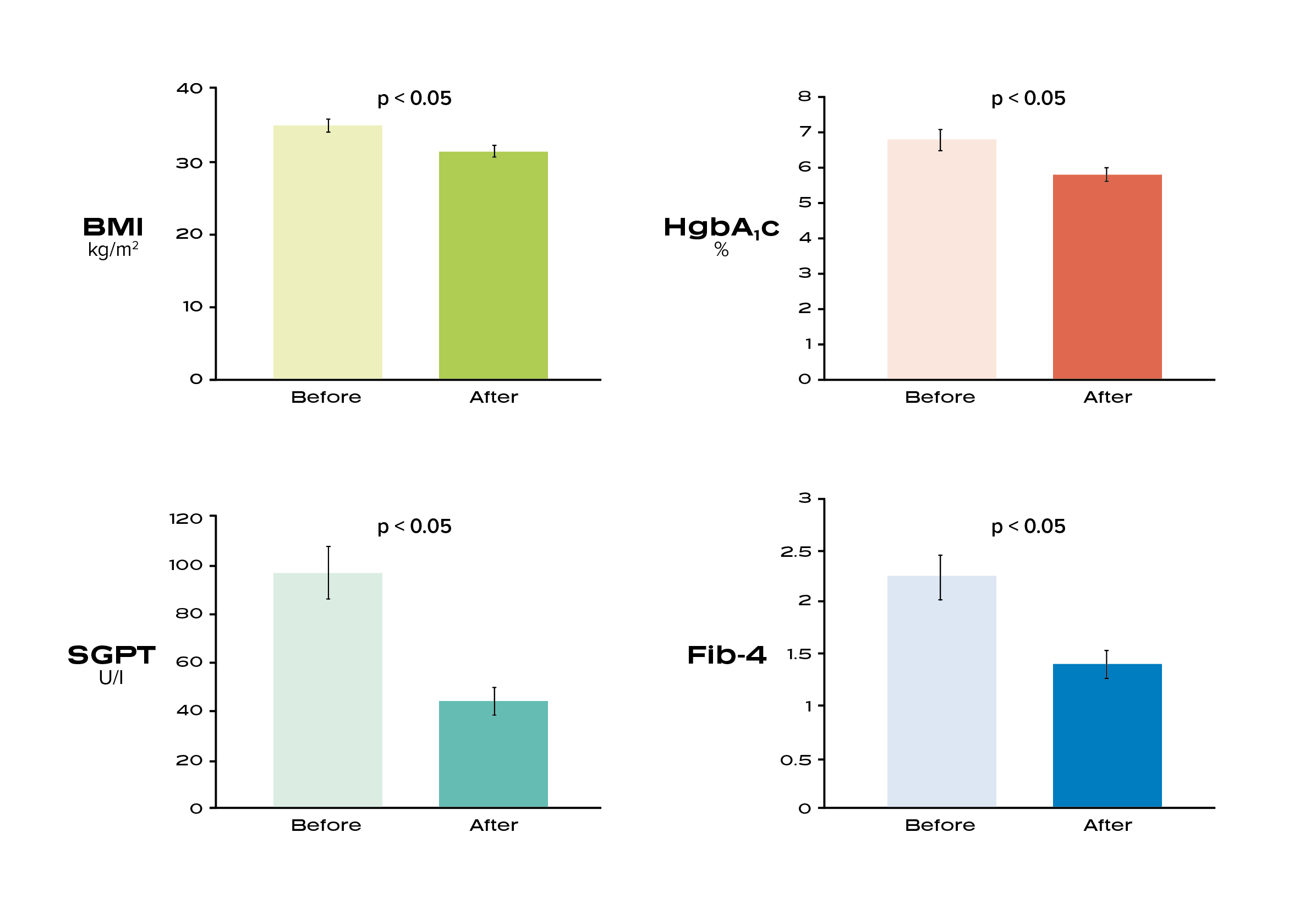
The goal of this study was to examine the impact of the Ideal Protein Protocol on metabolic parameters and markers of liver disease in patients with non-alcoholic steatohepatitis.
The findings highlight the beneficial effects of the Ideal Protein Protocol on liver enzymes and a marker of liver fibrosis among a group of patients with NASH⁸’⁹
Experts estimate that the prevalence of NASH is up to 12%, over 16 million US adults, with estimates of a 63% increase by year 2030. ¹⁰
⁸ Belopolsky Y, Khan MQ, Sonnenberg A, Davidson DJ, Fimmel CJ. Ketogenic, Hypocaloric Diet Improves Nonalcoholic Steatohepatitis. J Transl Int Med. 2020;8(1):26-31. Published 2020 May 9. doi:10.2478/jtim-2020-0005
⁹ Promrat K, Kleiner DE, Niemeier HM, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010;51(1):121-129. doi:10.1002/hep.23276
¹⁰ Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67(1):123-133. doi:10.1002/hep.29466
Dr. Davidson is a member of Ideal Protein’s Medical Advisory Board.
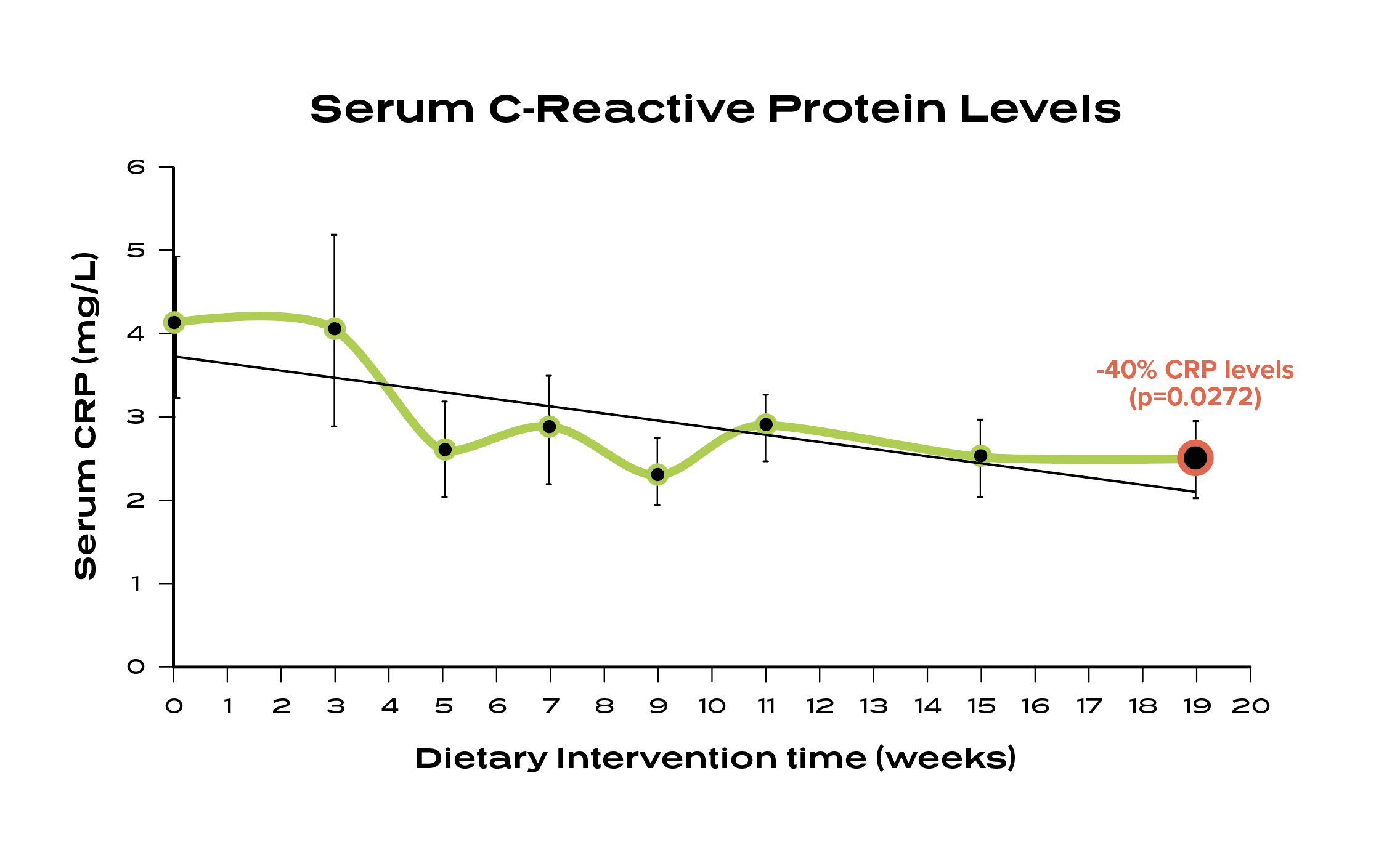
A 19-week study with the Avera Cancer Institute reported a 40% reduction in C-reactive protein for patients who completed the Ideal Protein Protocol. The study also reported a rapid decline in resting fasting insulin and a mean weight loss of 19.9% body fat. ⁶
Studies show increased CRP levels are associated with a higher risk for inflammatory conditions. ⁷
⁶ Bohlen, Krista & Krie, Amy & Hu, Yueshan & Ageton, Cheryl & Nickles, Heidi & Norfolk, Daniel & Kittelsrud, Julie & Thomes, Reggie & Fahrendorf, Adam & Muth, Jessica & Rojas-Espaillat, Luis & Davies, Gareth. (2013). Low Carbohydrate Dietary Intervention Improves Insulin, Hormonal Levels and Inflammatory Markers in Early Stage, Postmenopausal Breast Cancer Survivors. Cancer Research. 73. 10.1158/0008-5472.SABCS13-PD2-5.
⁷ Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;112(2):299. doi:10.1172/JCI200318921C

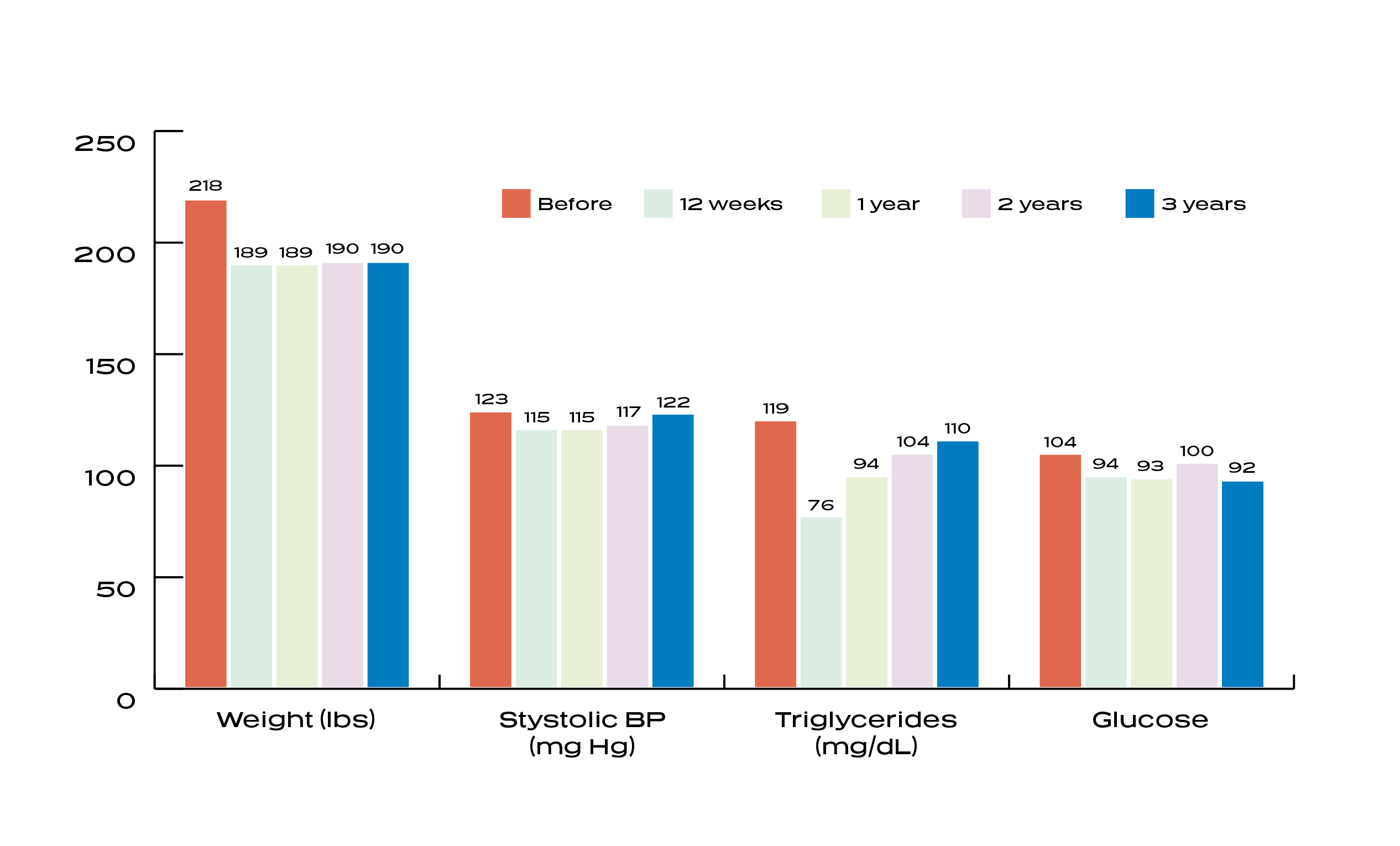
A study conducted by Aspirus, reported that after 3 years, participants who completed the Ideal Protein Protocol maintained an average weight loss of 12.8%, resulting in an 18% reduction in overall average claim care costs, saving an average of $916.97 per participant, per year. ²
A study published by The American Journal of Clinical Nutrition reports that if individuals can succeed at maintaining their weight loss for 2 or more years, they can reduce their risk of subsequent regain by nearly 50%.³
² Effect of The Ideal Protein Weight Loss Protocol on Employee Health Care Costs, By: Timothy Logemann, MD; David K. Murdock, MD; Kelly O’Heron, RD
³ Rena R Wing, Suzanne Phelan, Long-term weight loss maintenance, The American Journal of Clinical Nutrition, Volume 82, Issue 1, July 2005, Pages 222S, 225S, https://doi.org/10.1093/ajcn/82.1.222S
According to a study conducted and published by Aspirus, an eight-hospital health system in Wisconsin and Michigan, entitled Effect of the Ideal Protein Weight Loss Method on Weight Loss and Metabolic Parameters,¹ 233 patients completed at least 12 weeks of the Protocol. The 12-week results were presented at the Cleveland Clinic’s 9th Annual Obesity Summit and at the Annual Scientific Meeting of the National Obesity Society.
Our peer-reviewed, published research demonstrates that, among patients who completed the study, metabolic health can be improved in as little as 12 weeks.
15%↓
BMI
8.6%↓
Blood
Pressure
14%↓
Total Body Weight*
14%↓
Cholesterol
86%
Dieter
Compliance
14%↓
Fasting
Glucose
45%↓
Triglycerides
13%↓
LDL
Study Concludes: The Ideal Protein Protocol produces improvements in blood pressure, lipid profile, particularly in regard to triglyceride levels and fasting glucose levels. The findings suggest that due to the successful weight loss reported, the Protocol could help with cardiovascular risk.
* Total Body Weight -3.5lbs/wk for men and -2.4lbs./wk for women
¹ Effect of the Ideal Protein Weight Loss Method on Weight Loss and Metabolic Parameters By: Timothy Logemann, MD; David K. Murdock, MD, MS; Kelly O’Heron, RD & Adam Hoffmann
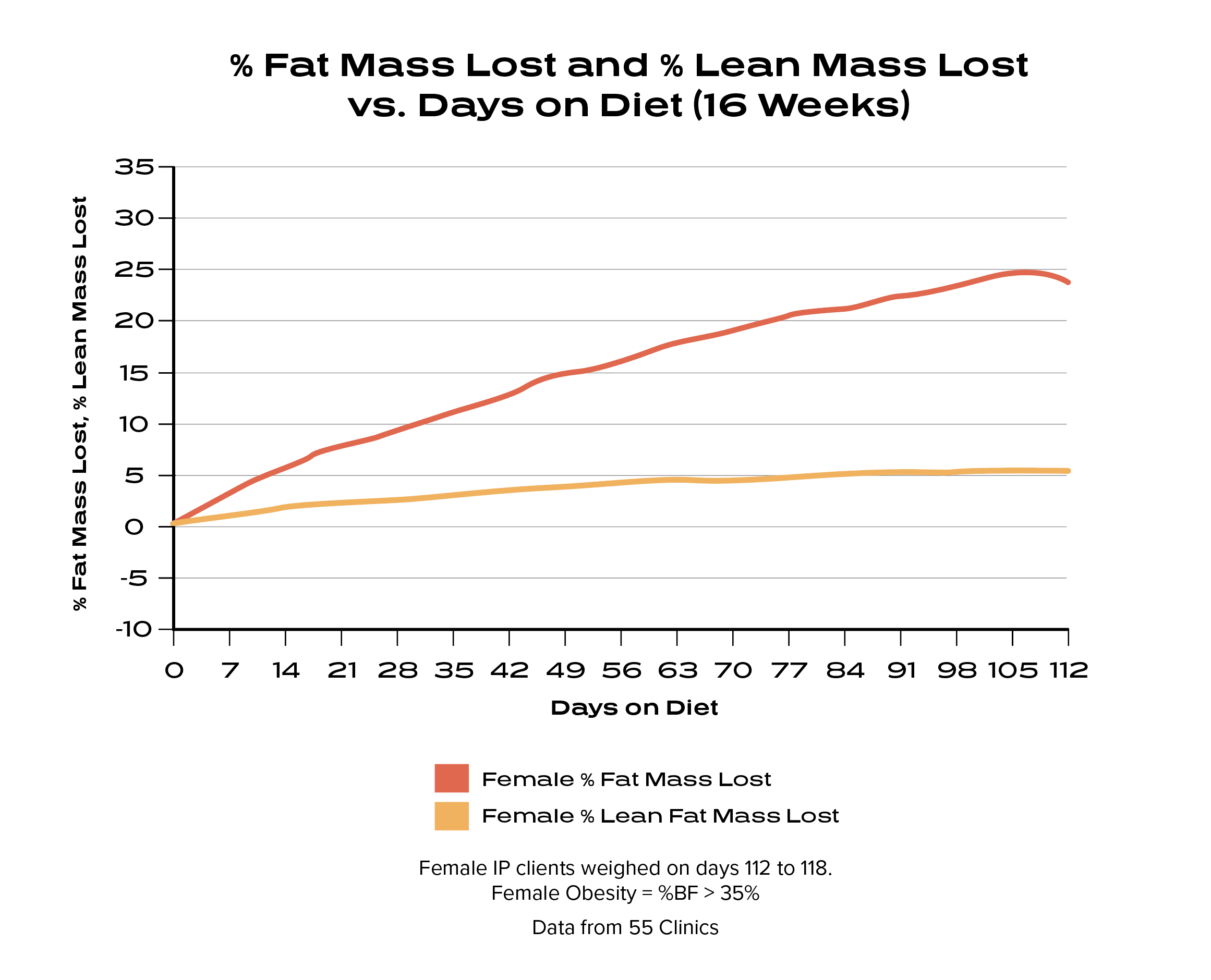
After 16 weeks on the Ideal Protein Protocol, males lost an average of 25% fat mass while preserving 98% lean body mass and females lost an average 24% of fat mass while preserving 95% lean body mass.⁴
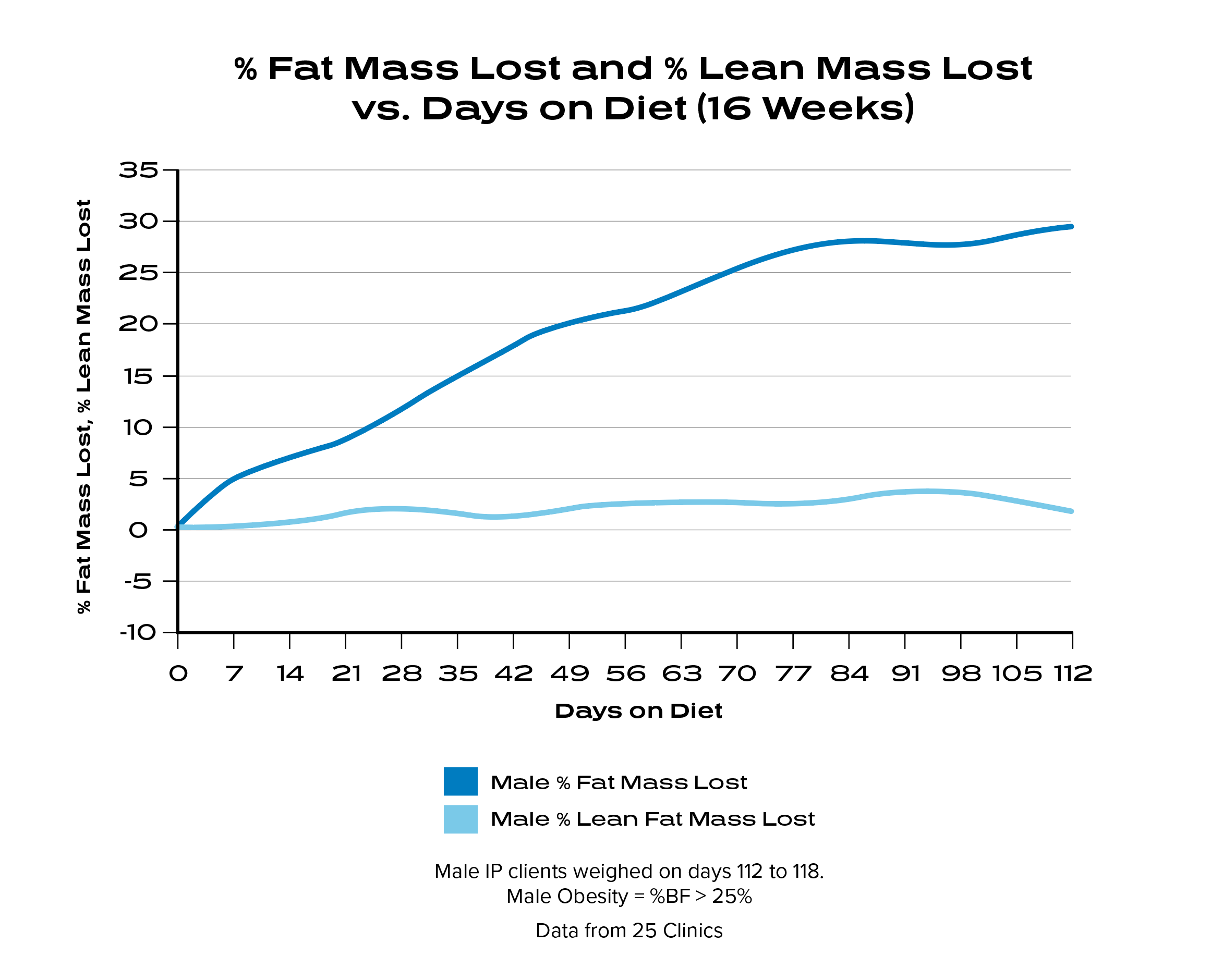
A 2014 Obesity Review states: “Maximizing fat loss while preserving lean tissue mass and function is a central goal of modern obesity treatments. A widely cited rule guiding expected loss of lean tissue as fat-free mass (FFM) states that approximately one-fourth of weight loss will be FFM (i.e. ΔFFM/ΔWeight = ∼0.25), with the remaining three-fourths being fat mass.” 5
⁴ Frank Douglis, MD, Ideal Protein Data Analysis, 2016.
⁵ Heymsfield SB, Gonzalez MC, Shen W, Redman L, Thomas D. Weight loss composition is one-fourth fat-free mass: a critical review and critique of this widely cited rule. Obes Rev. 2014;15(4):310-321. doi:10.1111/obr.12143
Dr. Douglis is an Executive Medical Board Member and Chief Medical Advisor for Ideal Protein.






